Malaria:
Malaria, a vector-borne disease transmitted by Anopheles mosquitoes, has been a major public health challenge for our country for the past many decades. Various national programmes targeting its elimination have met with limited success. Though Kerala had controlled the disease in the early 1970s, Malaria incidents still exist as a public health challenge. The problem has recently aggravated because of the presence of large-scale population movement from malaria endemic States. The proportion of falciparum malaria, the more severe form of the disease also exists in Kerala. Though the elimination of the Indigenous form of Malaria has been included in the SDG targets by the State, the issues in its fulfilment are many. Rapid urbanisation, extensive infrastructure development in many districts, uncontrolled construction works in urban areas and climate related changes in the life cycle of mosquitoes are big hurdles in the attainment of the SDG goals. Annual cases of malaria in Kerala are less than 500 and the number of deaths reported is also very low. Kasaragod District has persistently had a high number of malaria cases, over many years, because of its proximity to the highly endemic districts of Karnataka. The movement of fishermen along the western coast of our State is a potential threat to the spread of malaria along the coastal districts. In 2023 number of cases reported was 563 and death reported was 7. In 2024, up to August, 597 cases and 5 deaths were reported. The number of malaria cases and deaths has been increasing over the years in Kerala. Number of cases and death from 2019 to 2024 (August 31) is given below:
|
Name of Diseases
Case
|
2020
|
2021
|
2022
|
2023
|
2024 (Upto Aug 31)
|
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
|
Malaria
|
267
|
1
|
309
|
1
|
438
|
0
|
563
|
7
|
597
|
5 |
|
Source: Directorate of Health Services
|
Japanese Encephalitis (JE):
This is a form of encephalitis, an inflammatory disease of the brain and its coverings, and is also a mosquito-borne infection. Kerala is more prone to this disease because of the presence of large paddy fields as the virus responsible for the disease is spread by Culex mosquitos, which breeds abundantly in water-logged areas of paddy fields. The peculiar nature of the Culex mosquito to breed in contaminated water increases the potential threat in other areas as well. The role of migratory birds in the transmission of JE is an extra risk for Kerala because our State has many sanctuaries for migratory birds. But since there is an effective vaccine against JE, we can be optimistic in its control programme, by strengthening the JE vaccination. In 2023, seven cases and two deaths were reported. Six cases and three deaths have been reported in 2024 (up to August 31). The number of JE cases and deaths is showing an increasing trend in Kerala. Details of cases and deaths from 2019 to August 31, 2024, are given below:
|
Name of Diseases
|
2020
|
2021
|
2022
|
2023
|
2024 (Upto Aug 31)
|
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
|
Japanese Encephalitis (JE)
|
0
|
0
|
0
|
0
|
2
|
0
|
7
|
2
|
6
|
3
|
|
Source: Directorate of Health Services
|
Water Borne Diseases:
The waterborne disease is mainly attributed to the unavailability of safe drinking water in many parts of the State especially in tribal and coastal areas. Unhygienic drinking water sources such as wells, pump houses, water supplied through tanker lorry, leaks in public water supply pipes and the consequent mixing of foul water with drinking water, dumping of wastes including sewage in water sources, use of commercial ice in preparation of cool drinks and using unsafe water in preparation of welcome drinks are some reasons for the spread of water-borne diseases. The Health Department has implemented a programme called “Jagratha” since November 2017 for the prevention and control of communicable diseases. There has been a considerable increase in incidents of typhoid, Hepatitis –A, Cholera and ADD (diarrhoea) in Kerala since 2020. Details of cases and deaths due to waterborne diseases of Acute Diarrhoeal Diseases (ADD), typhoid and Hepatitis from 2019 to 2024 August 31 are given below:
|
Prevalence of water borne diseases in Kerala
|
|
Name of Diseases
Case
|
2020
|
2021
|
2022
|
2023
|
2024(Aug 31)
|
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
Case
|
Death
|
|
Hepatitis-A
|
464
|
2
|
114
|
0
|
231
|
2
|
1073
|
11
|
4610
|
53
|
|
Cholera
|
2
|
0
|
1
|
0
|
1 |
0
|
26
|
0
|
35
|
1
|
|
Typhoid
|
16
|
0
|
30
|
0
|
55
|
0
|
102
|
0
|
109
|
0
|
|
ADD (Diarrhoea)
|
250788
|
1
|
238227
|
3
|
466211
|
2
|
485929
|
2
|
392486
|
12
|
|
Source: Directorate of Health Services
|
HIV/AIDS:
Kerala State Aids Control Society is the pioneer organisation in the State working to control the spread of HIV as well as strengthen the State’s capacity to respond to HIV/AIDS. In Kerala, the prevalence of HIV/AIDS is 0.41 per cent (4.95 per cent in 2011) among injecting drug users (IDU) which is 6.26 per cent at the national level. It is 0.23 per cent (0.36 per cent in 2011) among men having sex with men (MSM) which is 2.69 per cent at the national level and 0.10 per cent (0.73 per cent in 2011) among Female Sex Workers (FSW) which is 1.56 per cent in India in 2017. Among transgender, the HIV prevalence rate in Kerala is 0.16 per cent which is 3.14 per cent at the national level. HIV prevalence among migrants in India is 0.51 per cent (Source: Kerala State Aids Control Society). HIV estimates in India and Kerala based on India HIV Estimates 2023 are given below:
|
HIV estimates in India and Kerala
|
|
Sl. No.
|
Particulars
|
Kerala
|
India
|
|
1
|
Percentage of adult HIV prevalence (15–49 yrs)
|
0.07
|
0.2
|
|
2
|
Total number of People Living with HIV (in lakhs)
|
0.24
|
25.44
|
|
3
|
HIV incidence per 1,000 uninfected population
|
0.01
|
0.05
|
|
4
|
New HIV infections (in thousands)
|
0.33
|
68.45
|
|
5
|
Decline in new HIV infections since 2010 (%)
|
74.39
|
44.23
|
|
6
|
AIDS-related mortality per 100,000 population
|
0.81
|
2.61
|
|
7
|
AIDS related deaths (in thousands)
|
0.29
|
35.87
|
|
8
|
Decline in AIDS related deaths since 2010 (%)
|
71.54
|
79.26
|
|
9
|
Need of services for Elimination of Vertical Transmission of HIV (in thousand)
|
0.1
|
19.96
|
| 10 |
Final Mother-to-Child Transmission rate of HIV (%) |
|
11.75 |
|
Source: India HIV Estimates 2023, NACO, MH&FW
|
Coronavirus Disease (COVID-19):
The first case of Covid-19 in India was reported in Kerala on January 30, 2020. Kerala adopted a multi-pronged strategy in dealing with the pandemic even before the first Covid-19 confirmed case was reported. Kerala’s response to COVID-19 started much earlier than March 11, 2020, when the Director General of the World Health Organisation (WHO) characterized COVID-19 as a pandemic. The containment strategies were well in place when the first case was reported. From the beginning of COVID-19 control activities, the private hospital engagement team was working in close liaison with the district private hospital engagement nodal officers, private hospital managements and the Indian Medical Association. Kerala Medical Services Corporation Limited has played the most critical role in the ambulance services by managing the Kaniv-108 ambulances to mobilise the COVID-19 suspects/ patients from their houses/exit points to the isolation facilities. During the coronavirus outbreak in Kerala, it was decided to provide psychosocial support ‘Ottakkalla Oppamundu’ to the persons in quarantine/isolation and their family members. State-level trainings were conducted exhaustively and elaborately covering all staff working in the health sector. Ward-level teams were active in all Panchayats and were ensuring daily calls and visits to the homes of the elderly. A series of mass media campaigns were being conducted for COVID-19 awareness from the beginning of 2020. Health Department launched e-Sanjeevani telemedicine services in Kerala on June 10, 2020. They were providing services in a centralized manner and DISHA is the State’s hub managing the telemedicine activities for the State.
Non-Communicable Diseases (NCD):
Common non-communicable diseases causing great threat to a healthy life are diabetes, hypertension, cardio vascular diseases, cancer and lung diseases. Unless interventions are made to prevent and control non-communicable diseases, their burden is likely to increase substantially in future because of ageing population and changes in life style. Considering the high cost of medicines and longer duration of treatment, this constitutes a greater financial burden for low income groups. Rapid urbanisation, drastic lifestyle changes, heavy dependency on alcohol and tobacco, affinity for white collar jobs, unhealthy eating patterns, low priority for physical exertion, high levels of stress in all strata of population are some of the reasons contributing to the prevalence of non-communicable diseases in the State.
Incidents of obesity, hyper lipedemia, heart attack and stroke are also high. Cancer mortality is extremely high among males in Kerala compared to national average. A survey conducted by Achutha Menon Centre for Health Science Studies, Thiruvananthapuram reveals one out of three has hypertension and one out of five has diabetes. The study also revealed that the level of normalcy attained for blood sugar and blood pressure even after early detection and management is significantly low compared to the standards.
Even though the State has witnessed a steep decrease in the use of tobacco in the Global Adult Tobacco Survey 2016 with the prevalence dipping to 12 per cent from 21 per cent, the increasing consumption of alcohol is affecting the health sector with prevalence rate as high as 44 per cent and age of starting coming down every year. The unhealthy dietary practices and lack of physical exercise in all sections of the population irrespective of the age and economic status has contributed to the rise in lifestyle diseases resulting in 52 per cent of total deaths in the productive age group between 30 and 70 being due to one or other cause of NCD.
(Source: DHS)
Prevalence of Anaemia:
The findings of the NFHS-5 (2019-2021) reveal that there has been an increase in the prevalence of anaemia among women and children compared to NFHS-4, 2015-16. Kerala is the only State to have recorded a prevalence of less than 40 per cent in all targeted age groups. Anaemia Mukt Bharat (AMB) strategy was launched in 2018 with the objective of reducing anaemia prevalence among children, adolescents and women in reproductive age group. Anemia Free Kerala aims to strengthen the existing mechanisms imparted as part of Anemia Mukth Bharth and foster State specific newer strategies for tackling anaemia. Details of Anaemia prevalence in Kerala as per NFHS-5 compared to NFHS-4 is given below:
Anaemia prevalence in Kerala as per NFHS-5 compared to NFHS-4
|
Indicator
|
NFHS-4
|
NFHS-5
|
|
Children age 6-59 months who are anaemic (<11.0 g/dl) 22 (%) percentage of children in the said age group with a haemoglobin concentration less than 11 g/dL
|
35.7
|
39.4
|
|
Non-pregnant women age 15-49 years who are anaemic (<12.0 g/dl) 22 (%)
|
34.7
|
36.5
|
|
Pregnant women age 15-49 years who are anaemic (<11.0 g/dl) (%) percentage of women with a haemoglobin concentration less than 11 g/dL
|
22.6
|
31.4
|
|
All women age 15-49 years who are anaemic (%)percentage of women with a haemoglobin concentration less than 12 grams per decilitre (g/dL)
|
34.3
|
36.3
|
|
All women age 15-19 years who are anaemic 22 (%)
|
37.8
|
32.5
|
|
Men age 15-49 years who are anaemic (<13.0 g/dl) 22 (%)
|
11.8
|
17.8
|
|
Men age 15-19 years who are anaemic (<13.0 g/dl) 22 (%)
|
14.3
|
27.4
|
|
Source: NFHS 5, NFHS 4
|
Cancer:
According to World Health Organisation, global cancer burden is increasing with 20 million new cases of cancer and 9.7 million deaths in 2022. In India, approximately one in nine people is expected to face a cancer diagnosis in their lifetime. Lung cancer is ranked highest among males and breast cancer in females (source: Indian Council for Medical Research).
Cancer is a major non communicable disease in Kerala. Apart from Medical Colleges, Regional Cancer Centre, Malabar Cancer Centre and Cochin Cancer Research Centre are the major hospitals in Government sector which offer treatment for cancer patients. Apart from these institutions all the major Government hospitals provide cancer treatment. Delay in early detection, huge treatment cost, minimal treatment centres and lack of awareness contribute to high mortality of the disease.
The details regarding cases registered in RCC in the last 10 years show that the highest number of new cases registered was in 2017-18(16443). The lowest was in 2020-21(11,191) which was 27.7 per cent lower than the previous year and it may be attributed to Covid-19 pandemic. In 2022-23, the new cases registered were 15,324 and that in 2023- 24 were 15,131, indicating 1.3 per cent decrease from previous year. New cases registered in RCC from 2014-15 to 2023-24 are given below:
|
Hospital Statistics 2023-24
|
|
IP Bed strength
|
298
|
|
Operational bed
|
286
|
|
Average OP per day
|
878
|
|
Average admissions per month
|
1069
|
|
Bed occupancy rate
|
95.97 per cent
|
|
Source: RCC, Thiruvananthapuram
|
Health Care Institutions:
In Kerala modern medical services are offered by the Directorate of Health Services (DHS) and the education sector concerned is dealt with by the Directorate of Medical Education (DME).
Health Care Institutions under DHS:
At present there are 1,288 health institutions with 38525 beds, 6545 doctors, 14378 nursing staff and 7312 paramedical staff under Health Services Department consisting of 849 PHC/FHCs, 226 CHCs/Block FHCs, 88 taluk headquarters hospitals, 18 District hospitals, 18 general hospitals, 3 mental health hospitals, 10 women and children hospitals, 3 leprosy hospitals, 14 TB hospitals, 2 other speciality hospitals and 57 other hospitals. PHCs/ FHCs are institutions providing comprehensive primary care services including preventive care and curative care. CHCs/ Block FHCs and taluk level institutions form the basic secondary care institutions. District hospitals, general hospitals and maternity hospitals provide specialty services and some super specialty services. Category-wise major medical institutions and beds in Kerala, details of IP and OP cases, major and minor surgeries conducted DHS during 2023-24 and 2024-25 and medical and paramedical personnel under DHS are given Table 1, Table 2, Table 3.
District-wise Distribution of Hospital Beds in Kerala:
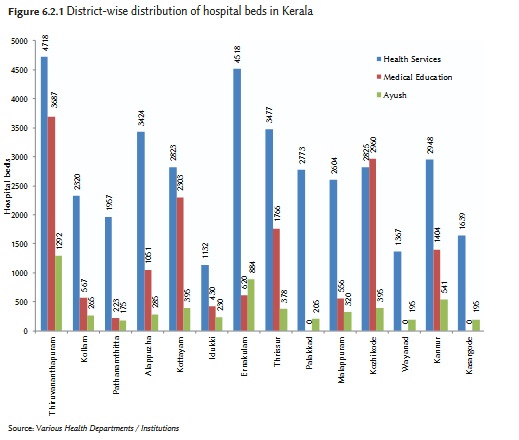
District-wise distribution of hospital beds in Kerala is given below. Thiruvananthapuram and Ernakulam districts have a higher number of beds as compared to other districts while Kasaragod, Idukki and Wayanad districts have a lesser number of beds. The bed population ratio in Kerala is 1:602 and it is 1:666 for modern medicine alone. The average doctor bed ratio in Kerala is 1:4 and it is 1:5 for modern medicine alone. The doctor-population ratio in Kerala is 1:2592. The population here is estimated for the year 2021. These figures reflect the status of the Government sector only and the figures will be much better if the private sector is also considered.
District-wise Distribution of Hospital Beds in Kerala
Comparative Analysis of Major Communicable Diseases 2009-23
NOROVIRUS INFECTION
Health Indicators Definitions
⇒ Prevalence of principal communicable diseases during 2013-2017(up to October)
⇒ 100 Core Health Indicators 2015
⇒ 100 Core Health Indicators 2018
Source: Economic Review 2011-2024